A) Acute pyelonephritis
B) Aspiration pneumonia
C) Incisional infection
D) Pulmonary embolism
E) Septic pelvic thrombophlebitis
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 70-year-old woman comes to the office due to vulvar pruritus. The patient has had increasing pruritus over the past 4 months that has not improved with topical emollients. She has no pelvic pain, vaginal bleeding, or abnormal vaginal discharge. The patient had similar symptoms 20 years ago, for which she was prescribed a corticosteroid cream that resolved the symptoms. She has not been sexually active for the last 10 years. The patient has hypercholesterolemia and type 2 diabetes mellitus. Her last Pap test with HPV cotesting was normal 5 years ago. Blood pressure is 132/78 mm Hg and pulse is 84/min. BMI is 32 kg/m2. On pelvic examination, there is a firm, white plaque with overlying excoriations on the left labium majus. Mild atrophy of the bilateral labia minora is noted, and the vagina has minimal rugation but no lesions. Which of the following is the best next step in management of this patient?
A) High-dose topical corticosteroids
B) Laser ablative therapy
C) Oral antifungal medication
D) Topical estrogen cream
E) Trichloroacetic acid therapy
F) Vulvar biopsy
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 60-year-old woman comes to the office for a breast cancer follow-up visit. The patient recently underwent a right mastectomy for a node-negative, estrogen- and progesterone-receptor-positive tumor. She was started on an aromatase inhibitor for adjuvant therapy; however, the medication was discontinued due to severe fatigue and poor sleep. As a result, she is scheduled to begin a 5-year course of adjuvant therapy with tamoxifen. The patient has no other chronic medical conditions and her only medication is a daily multivitamin. Her last menstrual period was 5 years ago. The patient's father had a myocardial infarction at age 65; family history is otherwise noncontributory. She does not use tobacco, alcohol, or illicit drugs. Vital signs are stable. BMI is 21 kg/m2. The patient has many concerns about tamoxifen therapy and asks about potential side effects. Which of the following is the patient at greatest risk for developing due to tamoxifen therapy?
A) Decreased bone density
B) Dysplasia of the cervical transformation zone
C) Ectopic endometrial tissue in the myometrium
D) Hyperplasia of the endometrium
E) Intimal thickening of the coronary arteries
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 24-year-old woman comes to the office for evaluation of dysuria and hematuria. For the past 3 days, the patient has had burning with urination and blood-tinged urine. She has had no fever, involuntary loss of urine, or postvoid dribbling. The patient has no bladder pain between voidings. She has had similar episodes for the past 6 months, starting a few days prior to menses. The symptoms usually resolve spontaneously, and she is asymptomatic for a few weeks before symptoms recur. The patient has no other medical conditions and takes no daily medications. Temperature is 36.7 C (98.1 F) , blood pressure is 110/80 mm Hg, and pulse is 76/min. BMI is 21 kg/m2. The lower abdomen is slightly tender to palpation with no rebound or guarding. There is no costovertebral angle or flank tenderness. On pelvic examination, the bladder is tender to palpation of the anterior vaginal wall. There is no urethral discharge. Urinalysis results are as follows:  Urine culture is negative. Which of the following is the most likely diagnosis in this patient?
Urine culture is negative. Which of the following is the most likely diagnosis in this patient?
A) Endometriosis
B) Interstitial cystitis
C) Nephrolithiasis
D) Recurrent urinary tract infection
E) Urethral diverticulum
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 32-year-old primigravid woman at 21 weeks gestation comes to the office due to increased vaginal discharge. The discharge started a week ago and initially was clear but turned slightly bloody today. The patient has had no abdominal pain or heavy vaginal bleeding. The patient has no chronic medical conditions and has had no prior surgeries. Temperature is 36.8 C (98.2 F) , blood pressure is 96/62 mm Hg, and pulse is 92/min. BMI is 19 kg/m2. The uterus is nontender, fundal height is 19 cm, and fetal heart tones are 155/min. Speculum examination shows scant blood and discharge; a bulging bag with fetal parts is protruding through the cervix, which is dilated 4 cm. Microscopy of the vaginal discharge shows squamous epithelial cells and few leukocytes. Nitrazine testing is negative. Which of the following is the most likely diagnosis in this patient?
A) Abruptio placentae
B) Cervical insufficiency
C) Incomplete abortion
D) Preterm labor
E) Preterm prelabor rupture of membranes
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 26-year-old nulliparous woman comes to the office due to severe pain during sexual intercourse. The pain is "particularly unbearable" with deep penetration, which has caused the patient to avoid sexual intimacy for the past few months. This has placed a significant strain on her relationship with her husband of 2 years, who has been her only sexual partner. They have been using condoms with lubrication during intercourse, but this has not improved the pain. Menses occur every 30 days, are painful, and last for 5 days with moderate bleeding. The patient has no chronic medical conditions and takes no daily medications. BMI is 24 kg/m2. Vital signs are normal. Speculum examination is normal. Which of the following is the most appropriate treatment for this patient's condition?
A) Cognitive-behavioral therapy
B) Combination oral contraceptives
C) Couples therapy and sex education
D) Pelvic floor physical therapy
E) Vaginal dilators
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 27-year-old primigravida at 18 weeks gestation comes to the office for a routine prenatal visit and an anatomy ultrasound. The patient feels well and has no concerns. She is accompanied by her mother as her husband was unable to get off work. The patient has no chronic medical conditions, and her only daily medication is a prenatal vitamin. Ultrasound shows a cephalic singleton fetus measuring at <10th percentile consistent with severe growth restriction. There are bilateral choroid plexus cysts, clenched fists, and a large ventricular septal defect. Amniotic fluid level is normal. The placenta is posterior and fundal. Which of the following is the most appropriate initial statement by the physician?
A) "Could I speak to you in private about my concerns with your ultrasound findings?"
B) "I'm sorry to tell you this, but it appears that the ultrasound findings are suggestive of a genetic anomaly."
C) "Let's schedule a follow-up visit to discuss the results when your husband can be here with you."
D) "There are some things about your ultrasound that I need to discuss with you; is it okay to do that now?"
E) "Would it be okay if your mother stepped out of the room so we can talk about your results?"
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 28-year-old woman, gravida 2 para 1, at 37 weeks gestation comes to the hospital due to severe abdominal and back pain. The patient's prenatal course has been uncomplicated, and her only medication is a daily prenatal vitamin. She had a prior cesarean delivery and is scheduled for a repeat cesarean delivery at 39 weeks gestation. Blood pressure is 90/60 mm Hg and pulse is 130/min. Fetal heart rate tracing is shown in the exhibit. Physical examination shows a palpable, irregular protuberance in the lower abdomen and moderate vaginal bleeding. Which of the following is the most likely cause of this patient's presentation?
A) Abruptio placentae
B) Normal labor with uterine fibroids
C) Placenta previa
D) Umbilical cord prolapse
E) Uterine rupture
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 32-year-old primigravida at 34 weeks gestation comes to the emergency department with right upper quadrant pain that started suddenly yesterday. The patient describes the pain as constant, severe, and stabbing. She has developed some rigors and chills but has had no confusion or mental status changes. The patient's only medication is a daily prenatal vitamin. Temperature is 38.7 C (101.7 F) , blood pressure is 136/84 mm Hg, pulse is 105/min, and respirations are 22/min. BMI is 38 kg/m2. Fetal heart rate monitoring has a baseline of 170/min with moderate variability. Scleral icterus is present. The uterus is nontender and measures at 34 weeks gestation. There is tenderness to palpation in the right upper quadrant with no rebound or guarding. Deep tendon reflexes are 2+. Bilateral lower extremities have 1+ pedal edema to the midcalf. Laboratory results are as follows:  Which of the following is the most likely diagnosis in this patient?
Which of the following is the most likely diagnosis in this patient?
A) Acute cholangitis
B) Acute fatty liver of pregnancy
C) HELLP syndrome
D) Intraamniotic infection
E) Preeclampsia with severe features
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 49-year-old woman, gravida 5 para 5, comes to the office due to urine leakage. Over the last 2 months, the patient has had constant urinary leaking, requiring her to wear a pad day and night. She has no dysuria, urgency, or vulvar pruritis. The patient has type 2 diabetes mellitus that is well controlled with oral medication. Two years ago, she received brachytherapy and external-beam pelvic radiation for cervical cancer. She had smoked a pack of cigarettes daily for 25 years but quit 6 years ago. BMI is 43 kg/m2. Pelvic examination shows no urethral leakage with Valsalva. There are postradiation changes and a pool of clear fluid in the vagina. Postvoid residual volume is 20 mL. Urinalysis results from catheterization are as follows:  Which of the following is the most likely cause of this patient's symptoms?
Which of the following is the most likely cause of this patient's symptoms?
A) Aberrant connection between the bladder and vagina
B) Decreased urethral sphincter muscle tone
C) Diminished contractility of the bladder detrusor
D) Excessive involuntary detrusor muscle spasms
E) External compression of the urethral outlet
F) Urethral hypermobility from weakened pelvic floor muscles
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 32-year-old woman, gravida 1 para 0, at 42 weeks gestation is admitted to labor and delivery for spontaneous rupture of membranes and contractions. The patient's pregnancy has been uncomplicated, and she has no chronic medical conditions and takes no medications. Blood pressure is 120/60 mm Hg, pulse is 78/min, and respirations are 12/min. Fetal heart rate monitoring shows a baseline of 130/min, absent variability, and recurrent late decelerations. Intrauterine resuscitation with maternal repositioning and oxygen administration does not improve the fetal heart rate tracing. The cervix is 4 cm dilated and 25% effaced on digital cervical examination. The patient is informed of the need for an emergency cesarean delivery due to significant risk for fetal asphyxia and death. However, she refuses to undergo cesarean delivery. Further discussion reveals that the patient fully understands the risks of refusing the procedure and continues to insist on a vaginal delivery. Which of the following is the most appropriate next step?
A) Proceed with emergency cesarean delivery because the fetal rights are more important than the patient's autonomy
B) Proceed with emergency cesarean delivery because there is evidence of fetal distress
C) Respect the patient's decision and proceed with vaginal delivery
D) Seek a court order forcing the mother to undergo emergency cesarean delivery
E) Seek out an alternative decision maker
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 34-year-old woman, gravida 2 para 1, at 34 weeks gestation comes to the office to establish prenatal care. The patient recently moved but had routine prenatal care in another state. She has had no contractions, vaginal bleeding, or leakage of fluid. Fetal movement is normal. The patient had a classical cesarean delivery at 25 weeks gestation due to eclampsia and fetal growth restriction. This pregnancy has been uncomplicated, and her only medications are a daily aspirin and prenatal vitamin. Blood pressure is 118/70 mm Hg. Fetal heart tones are 145/min and fundal height is 38 cm. Urine dipstick is negative for protein and glucose. An ultrasound is performed due to a uterine size/dates discrepancy. The ultrasound shows a posterior placenta, normal amniotic fluid volume, and a fetus in a frank breech presentation with an estimated fetal weight at the 50th percentile for gestational age. The patient would like to attempt a vaginal delivery with this pregnancy. Which of the following is the best next step in management of this patient?
A) Await spontaneous labor and perform internal podalic version
B) Induce labor for breech vaginal delivery at 40 weeks gestation
C) Perform external cephalic version at 36 weeks gestation
D) Repeat ultrasound in 2 weeks to determine mode of delivery
E) Schedule a cesarean delivery at 37 weeks gestation
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 26-year-old primigravid woman at 20 weeks gestation comes to the emergency department due to joint pain and swelling in her hands and feet over the past day. The patient reports good fetal movement and has no abdominal pain, bleeding, leakage of fluid, headaches, or visual changes. She has a history of systemic lupus erythematosus that was managed with hydroxychloroquine, which the patient stopped taking prior to conception. Blood pressure is 150/95 mm Hg; 5 minutes later, following rest in the lateral recumbent position, it is 140/95 mm Hg. Fetal heart rate by Doppler ultrasound is 145/min. Physical examination shows bilateral 2+ pitting edema of the legs and a red macular eruption on the cheeks. Laboratory results are as follows:  Serum electrolytes, liver function tests, and coagulation studies are within normal limits. Which of the following is the most likely diagnosis for this patient?
Serum electrolytes, liver function tests, and coagulation studies are within normal limits. Which of the following is the most likely diagnosis for this patient?
A) Gestational hypertension
B) HELLP syndrome
C) Hemolytic uremic syndrome
D) Preeclampsia
E) Systemic lupus erythematosus flare
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 63-year-old woman comes to the office for a routine annual examination. The patient feels well and has no concerns today. She underwent menopause at age 50 and has had no episodes of vaginal bleeding. The patient exercises multiple days a week and has no urinary or fecal leakage. BMI is 29 kg/m2. Blood pressure is 126/80 mm Hg and pulse is 80/min. Cardiopulmonary examination is normal. The abdomen is soft and nontender without palpable masses or hernias. On pelvic examination, vulvar atrophy is present, and the vagina appears pale and has minimal rugation but no lesions. The cervix appears normal and has no lesions or discharge. On Valsalva maneuver, there is a bulge of the anterior vaginal wall to the introitus. Postvoid bladder and renal ultrasound is normal. Which of the following is the best next step in management of this patient's pelvic organ prolapse?
A) Hormone replacement therapy
B) Pessary placement
C) Reassurance and observation
D) Surgical anterior vaginal wall repair
E) Urodynamic testing
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 34-year-old woman, gravida 1 para 1, comes to the office for infertility evaluation. She has been trying to conceive for the past year, but her cycles have become increasingly irregular, with the last menstrual period more than 3 months ago. Menses previously occurred every 27 days and lasted 4 days. The patient feels fatigued and has been waking up at night due to feeling too warm. She has been married for 6 years and has a 4-year-old daughter who was delivered vaginally without complications. The patient has hypothyroidism, for which she takes levothyroxine. She has no previous surgeries. The patient smokes a pack of cigarettes a day but does not use alcohol or illicit drugs. Both of her parents have type 2 diabetes mellitus. BMI is 24 kg/m2. Vital signs are normal. Pelvic examination shows normal external genitalia, a small mobile uterus, and normal bilateral ovaries. TSH is normal and a pregnancy test is negative. Which of the following would most likely be seen in this patient?
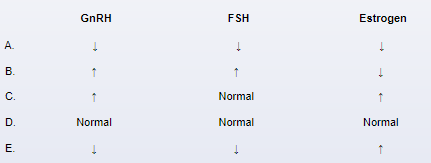
A) A
B) B
C) C
D) D
E) E
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 46-year-old woman comes to the office for evaluation of a vaginal mass. The patient has had intermittent vaginal pressure for the past 2 years that is now constant and worse with intercourse. She now notices a vaginal mass when voiding and sometimes sees light blood on the toilet paper after wiping. The patient has no chronic medical conditions. Her only surgery was a cervical conization 4 years ago; repeat Pap testing has since been normal. The patient had 3 uncomplicated vaginal deliveries in her 20s and a tubal ligation with her last delivery. She is recently divorced and has had 3 new sexual partners in the past year. The patient smokes a half pack of cigarettes daily and drinks 1-2 glasses of wine on the weekends. BMI is 23 kg/m². Vital signs are normal. On pelvic examination, there is a small erosion over the anterior vaginal wall but no lesions on the cervix. The cervix protrudes to the hymenal ring with Valsalva maneuver. The uterus is mobile and nontender, and there is a 2-cm pedunculated fundal uterine fibroid. Which of the following is the most likely contributing factor to this patient's clinical presentation?
A) Chronic tobacco use
B) Multiple pregnancies
C) Number of sexual partners
D) Prior cervical conization
E) Uterine leiomyomata
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 29-year-old woman, gravida 2 para 1, comes to the office for an initial prenatal visit. The patient is at 16 weeks gestation by her last menstrual period and has had no contractions, vaginal bleeding, or leakage of fluid. For the first 2 months of her pregnancy, the patient had daily nausea and vomiting that resolved without treatment. She has no chronic medical conditions and has had no previous surgeries. Her only medication is a daily prenatal vitamin that she started taking a few weeks ago. The patient does not use tobacco, alcohol, or illicit drugs. Vital signs are normal. BMI is 30 kg/m2. Cardiopulmonary examination is normal. The uterus measures 20 weeks gestation. Prenatal laboratory testing reveals that the patient's serum alpha-fetoprotein concentration is 3.8 multiples of the median (normal: <2.5) . Which of the following is the best next step in management of this patient?
A) CA-125 level
B) Fetal ultrasound
C) Increase prenatal vitamin dose
D) Quantitative β-hCG level
E) Repeat serum alpha-fetoprotein concentration
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 33-year-old woman, gravida 2 para 2, is evaluated on the postpartum floor due to low back and buttock pain. Yesterday, the patient had a forceps-assisted vaginal delivery after a prolonged induction of labor for preeclampsia with severe features. Epidural analgesia was removed immediately postpartum. Afterward, the patient began to develop low back and buttock pain. The pain is constant but worsens with sitting. She has no chronic medical conditions and did not have these symptoms during pregnancy. Temperature is 37.2 C (99 F) , blood pressure is 120/80 mm Hg, and pulse is 78/min. On examination, the uterine fundus is firm, and the perineum is intact with diffuse symmetric vulvar swelling. There is exquisite tenderness to palpation over the coccyx. There is no surrounding erythema. Deep tendon reflexes are 2+. Strength is 5/5 in the bilateral lower extremities. Which of the following is the best next step in management of this patient?
A) Blood cultures
B) Epidural blood patch
C) Erythrocyte sedimentation rate testing
D) MRI of the spine
E) Reassurance and analgesics
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 38-year-old woman at 6 weeks gestation comes to the office due to vaginal bleeding. The patient has had intermittent bleeding for the past week, which increases after intercourse. She has had no pelvic pain, nausea, or vomiting. Blood pressure is 124/68 mm Hg and pulse is 86/min. The abdomen is soft and nontender, without rebound or guarding. On pelvic examination, there is dark brown discharge pooling in the posterior vaginal vault. The cervix is closed, and there is a raised cervical mass that bleeds freely when manipulated with a swab. Ultrasound reveals a yolk sac and a 6-week intrauterine fetal pole with cardiac motion. Blood type is O, Rh positive. Which of the following is the best next step in management of this patient?
A) Ceftriaxone and azithromycin
B) Cervical biopsy
C) Endometrial biopsy
D) Expectant management only
E) Kleihauer-Betke test
F) Quantitative β-hCG level
Correct Answer

verified
Correct Answer
verified
Multiple Choice
A 20-year-old woman, gravida 2 para 2, is evaluated in the postpartum unit 8 hours after vaginal delivery. She is experiencing fatigue, perineal discomfort, and bloody vaginal discharge. The patient has voided 3 times since delivery. She was admitted to the hospital for rupture of membranes at 40 weeks gestation and, after a prolonged induction, had an uncomplicated vaginal delivery under epidural anesthesia with a second-degree laceration that was immediately repaired. The placenta delivered spontaneously, after which the patient had an episode of rigors and chills for 30 minutes that has not recurred. Estimated delivery-related blood loss was 300 mL; the patient received an oxytocin infusion for 4 hours after delivery. Temperature is 37.9 C (100.2 F) , blood pressure is 120/80 mm Hg, and pulse is 76/min. Pelvic examination shows an intact perineal repair with minimal bloody discharge and small blood clots on the perineal pad. The uterine fundus is firm, nontender, and palpable at the umbilicus. Which of the following is the best next step in management of this patient?
A) Broad-spectrum antibiotics
B) Oxytocin infusion
C) Pelvic ultrasound
D) Routine postpartum care only
E) Urinalysis and urine culture
Correct Answer

verified
Correct Answer
verified
Showing 181 - 200 of 469
Related Exams